Abstract
INTRODUCTION Allogeneic hematopoietic cell transplantation (allo-HCT) is a curative strategy for patients with high-risk hematological disorders. However, despite its curative potential, allo-HCT is still associated with transplant-related toxicity and mortality.
Graft-versus-host disease (GVHD) remains a matter of concern in allo-HCT. Post-transplant cyclophosphamide (PTCY) containing GVHD prophylaxis has changed the paradigm of haploidentical HCT (haplo-HCT). Secondary to its efficacy, the use of PTCY, combined with other immunosuppressant agents, is being expanded to matched sibling (MSD) and 10/10 HLA matched unrelated donor (MUD) allo-HCTs with notable success. Although the positive results derived from using PTCY out of the haplo-HCT setting, a standard of care has not yet been established.
PTCY, tacrolimus (TK) and mycophenolate mofetil (MMF) became our Institutional GVHD prophylaxis for peripheral blood (PB) haplo-HCT in 2013. In the subsequent years, the use of this prophylaxis was expanded to PB allo-HCT performed from mismatched unrelated donors, MUD and finally, from MSD. Due to the positive results derived from this prophylaxis, the use of MMF was abandoned, and PTCY-TK has become our Institutional GVHD prophylaxis for MUD and MSD PB allo-HCT.
This study reports the experience gained from using PTCY-TK in adults undergoing PB allo-HCT from MSD and MUD, and compares the results obtained from the use of this prophylaxis with those achieved from using other prophylaxis without PTCY.
METHODS This study included 272 consecutive adults with hematologic malignancies who underwent PB allo-HCT from MSD and MUD between June 2011 and November 2021. The study cohort was divided into two groups: PTCY-TK vs. no PTCY. PTCY-TK prophylaxis consisted of 50 mg/kg/day of PTCY IV given on days +3 and +4, and TK initiated on day +5 and maintained therapeutic until day +90. Other prophylaxis combined calcineurin inhibitors with methotrexate, MMF, or sirolimus. No patient received anti-thymocyte globulin. Retrospective data was updated in July 2022. Post-transplant follow-up was censored at 2 years.
RESULTS The following baseline characteristics between the 95 (35%) patients receiving PTCY-TK and the 177 (65%) receiving other prophylaxis were balanced: median age (54 vs. 53 years, P=0.986), KPS (<90%: 23.2% vs. 27.6%, P=0.448), HCT-CI (>3: 30.5% vs. 22.9%, P=0.189), and conditioning regimen intensity (MAC: 46.3% vs. 45.8%, P=0.930)]. However, patients older than 60 years (18.9% vs. 6.8%, P=0.002) and MUD allo-HCTs (82.1% vs. 40.1%) were more prevalent in the PTCY-group.
Overall, 270 patients engrafted. The median time to neutrophil and platelet engraftment was longer in the PTCY-TK group (21 vs. 16 days and 20 vs. 14 days, P< 0.001). The cumulative incidence function (CIF) of bacterial bloodstream infections at day +30, CMV reactivation, CMV disease, and BK hemorrhagic cystitis at day +180 were 49.3%, 45.0%, 6.2%, and 12.6% for patients receiving PTCY-TK and 13.6% (P<0.001), 59.1% (0.144), 8.8% (0.290) and 6.8% (P=0.134) for those who did not. No patient received letermovir.
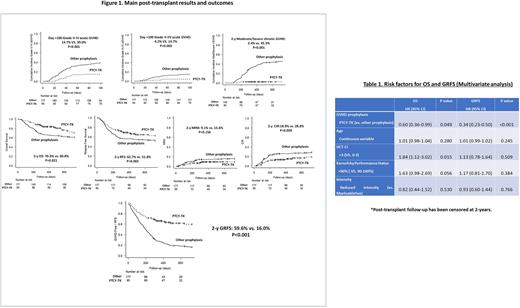
The CIF of grade II-IV and III-IV aGVHD at day +100 and mod/severe cGVHD at 2-years were 14.7%, 4.2% and 2.4% for patients receiving PTCY-TK, and 39.0% (P<0.001), 14.7% (P=0.003), and 45.3% (P<0.001) for those who did not. The duration of immunosuppression was shorter in patients receiving PTCY (188 vs. 272 days, P<0.001).
Compared with patients receiving other prophylaxis, patients receiving PTCY-TK had betterOS (2-y: 70.3% vs. 60.8%, P=0.021), a trend to higher RFS (2-y: 62.7% vs. 51.8%, P=0.065), comparable NRM (2-y: 9.1% vs. 15.6%, P=0.156) and inferior CIR (2-y: 18.9% vs. 28.8%, P=0.050). Moreover, the use of PTCY-TK significantly improved GVHD-Free/RFS (GRFS) (2-y: 59.5% vs. 16.0%, P<0.001) (Figure 1). Multivariate analysis reported in Table 1 confirmed that using PTCY-TK was a predictor for higher OS (HR 0.60, P=0.049) and better GRFS (HR 0.34, P<0.001).
CONCLUSIONS Using PTCY-TK for GVHD prevention is safe and more effective than other prophylaxis without PTCY for MSD and MUD PB allo-HCT.
Its use at our Institution has significantly decreased clinically relevant acute and chronic GVHD, allowing for faster discontinuation of the immunosuppression, and contributing to a reduction of disease relapse. Moreover, the use of PTCY-TK has increased post-transplant OS and specially, GRFS.
Disclosures
Cid:Pharm-Olam: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; MacoPharma: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Grifols: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Fresenius Kabi: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Sanofi: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Kawasumi Laboratories: Research Funding; Cerus: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; TerumoBCT: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Rosinol Dachs:BMS-Celgene: Honoraria; Amgen: Honoraria; Takeda: Honoraria; Sanofi: Honoraria; GlaxoSmithKline: Honoraria; Janssen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal